VIRAL HAEMORRHAGIC FEVERS / MedUrgent
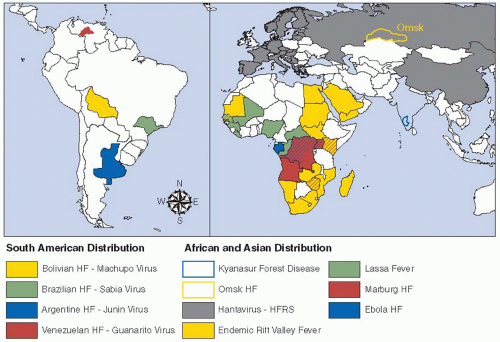
VIRAL HAEMORRHAGIC FEVERS
Viral Hemorrhagic Fever defines a
syndrome caused by 4 different families of RNA viruses. Though they have
constant features in common, yet there are particular clinical features
associated with different viruses. They can cause disastrous epidemics with
case fatality rate up to 50%.
Classification
1. Arenaviruses e.g. Guanarito, Junin, Machupo
and Lassa. They have rodent reservoir. Humans are infected by aerosols of
rodent excreta or other close contacts with rodents.
2. Bunyaviruses e.g. Rift Valley, Criean-Congo
and Hantaan. Transmission through mosquito bites, aerosols or contact with
blood of domestic animals, tick bite and rodent excreta.
3. Filovirus e.g. Ebola and Marburg. Mode of
transmission is by person to person through body fluids
4. Flaviviruses e.g. yellow fever, Dengue and Kyanasur forest disease. Mode of transmission is through mosquito and tick bites.
Clinical features
After contracting the disease, the incubation
period is 2 days to 3 weeks in average. VHF presents with fever, myalgia and
malaise for a few days and then the disease progresses with increased
prostration and specific organ involvement. Bleeding, jaundice, anuria, oedema,
conjunctival and retinal hemorrhages, CNS involvement. Shock and coma are
common terminal events.
Laboratory tests
Virology studies need highly equipped
laboratories. WHO should be informed in suspicious cases or epidemics.
Management
• Supportive therapy
DENGUE HAEMORRHAGIC FEVER
Dengue fever is caused by an arbovirus
transmitted to man by the daybiting Aedes mosquito. It has 4 serotypes (1, 2,
3, and 4) and there is no cross-immunity to these serotypes. Almost all
infections occur in children as adults are usually immune to the locally
circulating serotype of dengue virus.
Clinical Features
The disease starts apruptly 3–15 days after a
mosquito bite and presents as either:
1. Undifferentiated febrile disease with
severe headache, retro-orbital pain, blanching maculopapular rash, arthalgia,
and myalgia and may progress to encephalopathy.
2. A febrile illness with bleeding and shock.
WHO CASE DEFINITION OF DENGUE HAEMORRHORRAGIC FEVER
All these features must be present:
A. Fever
B. Hemorrhagic tendency:
at least one of the following:
i) Positive tourniquet test
II) Petechiae, purpura or ecchymosis
III) Bleeding
C. Thrombocytopenia
D. Evidence of plasma leakage:
i) Haematocrit>20% above average
II) Drop in haematocrit > 20% after volume
replacement
III) Clinical signs e.g. pleural effusion and
ascites.
WHO DEFINITION OF DENGUE SHOCK SYNDROME
All features of DHF plus evidence of circulatory failure:
a) Rapid and weak pulse
b) Narrow pulse pressure <20mm Hg
OR
a) Hypotension
b) Cold clammy skin and restlessness.
Laboratory tests
a) PCR
b) Immunocytochemistry
c) Antibodies: IgM (acute phase), IgG (rising titre)
d) Virus Culture.
Treatment
• No specific antiviral drug
• Conservative therapy
• IV fluids; Ringer lactate or colloids to
restore plasma losses.
• Blood transfusion
YELLOW FEVER
Yellow fever is caused by a flavivirus which
is transmitted by culicine mosquito. It causes explosive epidemics.
Clinical features
The disease starts abruptly 3-6 days after a mosquito bite with fever, chills, headache, myalgia, conjunctival congestion and relative bradycardia (Faget's sign). Jaundice, renal failure, bleeding, shock, coma and death may follow.
Treatment
• Supportive therapy. No specific treatment.
Ebola Hemorrhagic Fever
(Ebola Virus Disease)
The name Ebola is derived from a river in Congo (Zaire) where the first
epidemic reported in a village near this river in 1976. The disease is caused
by a Cilovirus called Ebolavirus that has 6 known species. Central and West
Africa are the mostly affected areas. The vector is the fruit bat that spreads
the virus through it's saliva and excreta, there for mostly affected people are
forest workers and miners. Nosocomial spread may occur where preventive
measures and precautions are not followed properly. Monkeys are similarly
affected and can act as an intermediate host. Epidemics occur usually at the
end of the rainy seasons.
Clinical Features
The virus is usually disseminated to all
organs causing necrosis and leading to a severe disease, though asymptomatic
cases have been reported. It starts as fever, fleeting maculopapular rash on
the face, abdominal pain due to the enlarging tender liver. Severe bleedings
and renal failure are signs of end-stage disease. Complications include
jaundice, hair loss, infection of testes and semen, eye infection and
hemorrhage, delirium, seizures and coma.
Laboratory diagnosis
-PCR
-ELISA
-Culture
Treatment
-There is no specific treatment
- Supportive therapy
-Monoclonal antibody therapy is on trial now
Prevention and Control
- Vaccination
- Avoid the habitat of bats e.g. dense
forests, mines, caves...etc
- Avoid eating of monkey meat or exposure to
it's blood or body fluids.
Chikungunya
Chikungunya is a Tanzanian word meaning "bends up". The disease is caused by an Arbovirus (CHKV) which is widely spread in Africa, India, Saudi Arabia, South East Asia and the islands of South West Indian Ocean. The vectors are Aedes egypti and Aedes albopictus. It affects humans, monkeys and baboons and appears usually in an epidemic form. Clinical Features Incubation period is 3 – 12 days . Epidemics occur mainly during wet seasons. It presents with fever and arthralgia which is usually symmetrical, affecting the small joints and may persist for months or years. Other features include severe back pain, generalized maculopapular rash, conjunctivitis and photophobia, mild hemorrhagic episodes especially in children, chills, nausea and vomiting. It is usually a self-limiting disease with a low fatality rate; however, complications do occur e.g. myocarditis and meningoencephalitis.
Laboratory diagnosis
- PCR
- High IgM
- Rising Hl or N antibody titer
- Culture
Treatment
- No specific treatment
- General symptomatic treatment
- Hydroxychloroquin for arthritis.
RELAPSING FEVERS
Relapsing fevers are caused by Borrelia spirochetes. The disease, if untreated, relapses repeatedly between afebrile intervals of 5-9 days. Borrelia recurrentis causes epidemics and it is transmitted by the human body lice pediculus humanous. Endemic Relapsing Fever is caused by other species of borrelia that are transmitted by ticks.
Clinical features
The incubation period is 4-17 days. Realpsing
fever starts with sudden high grade fever followed by headache, confusion,
myalgia, arthralgia, nightmares and prostration, bleedings, jaundice, chest
signs and hepatosplenomegaly. During pregnancy, the disease may lead to
abortion.
This phase ends with an afebrile period of 5-9
days, then, if untreated, it relapses. Death may occur due to myocarditis,
liver failure, severe bleeding, DIC, rupture of the spleen or secondary
bacterial infections. During epidemics Case Fatality Rate is 40% or even more.
Laboratory tests
- Blood film stained with Gimsa stain to see
the spirochetes.
- Full blood count shows pancytopoenia
Treatment
• A single dose of antibiotic is curative (tetracycline,
benzyl penicillin, erythromycin or chloramphenicol).
• General supportive measures.
Jarisch-Hexheimer Reaction
This syndrome occurs a few hours after
treatment of Relapsing Fever. It manifests as restlessness, high grade fever,
rigors, delirium, cough, diarrhea and vomiting, profuse sweating, shock and
pulmonary oedema secondary to myocarditis. Death rate is high if untreated.
Treatment includes cooling of temperature, circulatory support and digoxine.





Comments
Post a Comment